Introduction:
To Intact Villous Architecture Within the realm of histopathology, the term “intact villous architecture” holds significant importance, particularly in the evaluation of gastrointestinal tissues. It refers to the characteristic structural arrangement of villi, finger-like projections lining the mucosal surface of the small intestine. Understanding intact villous architecture is paramount in diagnosing various gastrointestinal disorders, particularly those affecting absorption and digestion processes. This discourse aims to unravel the intricacies of intact villous architecture, its clinical significance, and diagnostic implications.
1.Anatomy of Villi:
Before delving into intact villous architecture, it’s crucial to grasp the anatomy of villi themselves. Villi are small, finger-like protrusions that extend from the mucosal lining of the small intestine. Composed of a central core of connective tissue known as the lamina propria, villi are covered by a single layer of columnar epithelial cells. These epithelial cells play a pivotal role in nutrient absorption, as they are equipped with microvilli, further increasing the surface area for absorption.
2.Understanding Intact Villous Architecture:
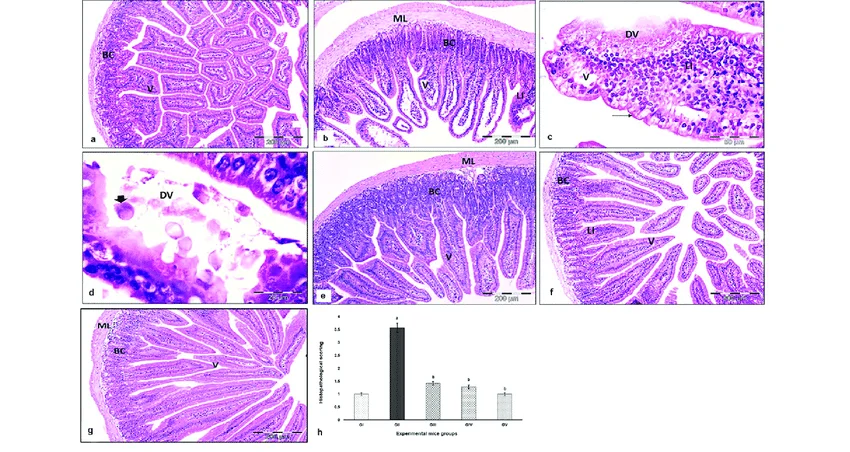
Intact villous architecture refers to the normal structural arrangement and appearance of villi within the small intestinal mucosa. Under microscopic examination, intact villi exhibit a uniform distribution, with well-defined finger-like projections extending into the intestinal lumen. The presence of intact villous architecture is indicative of normal gastrointestinal function, essential for efficient nutrient absorption and digestion processes.
3.Clinical Significance in Histopathology:
The assessment of intact villous architecture holds paramount importance in histopathological evaluations, particularly in the diagnosis of conditions such as celiac disease and tropical sprue. In celiac disease, an autoimmune disorder triggered by gluten consumption, the characteristic flattening of villi, known as villous atrophy, is a hallmark feature. Conversely, the preservation of intact villous architecture rules out significant mucosal damage, aiding in the exclusion of celiac disease and other malabsorptive conditions.
4.Diagnostic Implications:
The presence or absence of intact villous architecture serves as a diagnostic indicator in various gastrointestinal pathologies. In addition to celiac disease, conditions such as inflammatory bowel disease (IBD), microscopic colitis, and infectious gastroenteritis can affect villous morphology. Histopathological examination of intestinal biopsies allows pathologists to assess the degree of villous blunting or preservation, providing valuable insights into the underlying pathology and guiding clinical management decisions.
5.Histological Evaluation Techniques:
Histological evaluation of intact villous architecture involves the examination of tissue specimens obtained via endoscopic biopsy. These biopsies are typically obtained from the duodenum or jejunum, regions of the small intestine where villous architecture is most prominent. Tissue sections are stained using specialized stains such as hematoxylin and eosin (H&E), allowing for the visualization of cellular morphology and structural integrity.
6.Differential Diagnosis:
While the absence of intact villous architecture may suggest certain gastrointestinal pathologies, it is essential to consider a broad differential diagnosis. Other conditions, such as infectious agents (e.g., Giardia lamblia), autoimmune disorders (e.g., autoimmune enteropathy), and medication-induced enteropathy, can mimic the histological features of celiac disease or tropical sprue. A comprehensive clinical history, serological testing, and ancillary studies are often necessary to establish an accurate diagnosis.
7.Therapeutic Implications:
The recognition of intact villous architecture or villous atrophy has therapeutic implications, particularly in the management of celiac disease. For individuals with confirmed celiac disease, adherence to a strict gluten-free diet is essential to prevent further mucosal damage and promote villous recovery. Conversely, the identification of intact villous architecture in biopsy specimens may prompt clinicians to explore alternative etiologies for gastrointestinal symptoms, guiding appropriate treatment strategies.
Conclusion:
In conclusion, intact villous architecture serves as a cornerstone in the histopathological evaluation of gastrointestinal tissues, offering valuable insights into mucosal integrity and function. Whether assessing for the presence of celiac disease, tropical sprue, or other gastrointestinal pathologies, the recognition of intact villous architecture or villous atrophy carries significant diagnostic and therapeutic implications. Through meticulous histological examination and correlation with clinical findings, pathologists play a vital role in elucidating the complex interplay between mucosal morphology and gastrointestinal health.